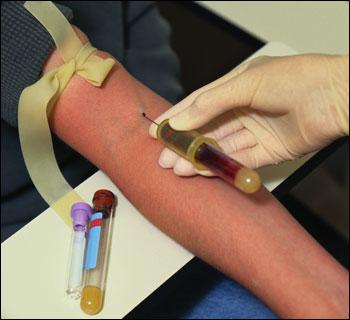
Venipuncture- This is a procedure that is carried out by nursing staff for medical and diagnostic purposes in most medical institutions. Venipuncture - insertion of a needle into a vein through the skin to draw blood or administer medicinal solutions, blood, blood substitutes. Venipuncture is the most common of all invasive interventions. Significant percentage of the total
the number of venipunctures is taking blood for laboratory tests.
Anatomy and physiology
Most often, venipuncture uses (to give a pic. From the atlas, denoting points all possible venopuncture sites) of the upper limbs, especially the anterior ulnar region, as they are numerous, easily accessible and their puncture causes minimal discomfort for the patient. These include:
Thus, elbow fossa veins are most commonly used ( rice 24), since they have a large diameter, lie superficially and are relatively little shifted. Metacarpous veins in most cases are well visualized and easily palpated, but their puncture is contraindicated in reduced skin turgor and depleted subcutaneous tissue. In some cases, the metacarpal veins are preferred to reduce the area of damage with possible extravasation in patients whose treatment uses cytotoxic substances or hypertonic solutions. Lower extremity veins are used for venipuncture.
Fig. 24. Anatomical location of the veins of the elbow area of a person.
In newborns and young children, venipuncture uses head veins, which they have well contoured, because the limb veins are very thin and it is often difficult to puncture them. It is necessary to remember about obtaining parental consent when performing this procedure.
Venipuncture should be avoided:
in the presence of signs of vein fibrosis;
in the presence of hematoma / edema;
in the presence of a local focus of infection / inflammation;
in the place of vascular access;
in place of a shunt or vascular graft.
After mastectomy, venipuncture should not be performed on the affected side due to possible impairment of lymphatic drainage. Guided also should be the choice of the patient and previous experience, which is taken into account in the course of obtaining patient consent.
Indications
Blood sampling for research.
The introduction of drugs.
Transfusion of blood and its components.
Intravenous anesthesia.
Introduction of contrast agents.
Extracorporeal detoxification.
Contraindications
Hypersensitivity to the drug.
The technical complexity of the puncture of peripheral veins.


Equipment:
Disposable rubber gloves.
Sterile balls.
Antiseptic.
Fig. 25. - Relevant blood collection containers.
The syringe of the required volume (for jet injection).
Necessary drug.
- Capacity for used needles.
Hypoallergenic plaster or bandage (if necessary).
For drip - refilled system.
Tripod for fixing bottles with drip.
This list is far from exhaustive; you should be guided by local protocols. In general practice, vacuum aspiration systems are widespread.
Syringes are also used quite often, but this increases the risk of damage to the vessel. In addition, a butterfly-type aspiration system may be used in certain specialized units. Some of these systems are equipped with a non-return valve, which is important for patients with thin veins. Regarding the need to treat the skin surface before venipuncture or peripheral catheterization, there are disagreements, however, it is common practice to thoroughly treat the skin with an appropriate solution.
Patient position
In preparing the patient for the procedure, he is explained the peculiarities, is calmed down whenever possible, his consent to the procedure is obtained, and they find out if he has allergic reactions to the substances that are supposed to be used. To stimulate the expansion of blood vessels and blood filling of the veins, you can use a tourniquet, however, the pressure must be such as to block the venous outflow without creating obstacles to the arterial blood flow. (give the scheme) The patient is asked to compress and unclench his fist. Remember that normal puncture of the vein can be painful and in patients with fragile veins to promote hematoma formation (since with intensive patting of the skin in the area of the vessels, histamine may be released).

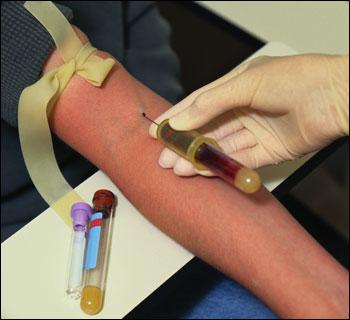
Algorithm for intravenous injection (Fig. 26)
prepare the equipment and prepare for the procedure;
specify patient data;
explain the procedure to the patient and get his consent;
make sure the patient is in a comfortable position;
process hands;
collect tools;
place the patient's hand on the roller;
Put a tourniquet on the limb (5-10 cm above the puncture site);
after palpation and selection of a vein for puncture, treat its area with alcohol (antiseptic) and let it dry;
Ask the patient to squeeze and open the fist as many times as possible.
Determine the needle insertion site.
Take the needle so that its cut is facing up, and inject the needle into the vein all at once. The direction of the needle is approximately 30 ° with respect to the vein.
If blood has emerged from the needle, then the needle is in the cavity of the vein.
Attach a syringe to the needle
Remove the harness.
Start the drug administration.
After the procedure, treat the skin with an antiseptic and tightly bandage the injection site for 30 minutes, or ask the patient to press the injection site firmly with a finger, or bend the elbow, pressing the cotton wool, for 5-10 minutes.
immediately discontinue the procedure if a hematoma is formed;
if necessary, apply a patch / bandage;
document the procedure;
make sure that the material is properly collected for analysis;
Factors complicating venipuncture
Excitement and fear of the patient.
Repeated puncture.
Sclerotic vein changes in elderly and senile patients.
"Floating" veins in a patient.
Thin veins (women, children).
Dehydration.
Fragile veins.
Long-term use of steroids.
Cachexia.
Complications and their removal
Injecting substance into the surrounding vein tissue. It is necessary to stop the introduction of the drug, if the drug has a high concentration, then you must enter the tissue saline or novocaine solution (0.25%) for the dilution of the drug.
The development of phlebitis, due to the toxic effects of the drug on the venous epithelium. Compresses with appropriate drugs (heparin, half-alcohol compress, physiotherapy).
Development of phlebitis and vein thrombosis with multiple venipuncture or prolonged presence of the needle in the vein lumen. Compresses with appropriate drugs (heparin, half-alcohol compress, physiotherapy).
Air embolism. Develops in the presence of about 1 ml 3 of air entering the vein. It is necessary to control the presence of air in the syringe - there should be no air embolism in your practice!
There may be complications in the form of piercing two vein walls with hematoma formation. (scheme to give) It is necessary to put a pressure bandage, and then compresses with appropriate drugs (heparin, half-alcohol compress, physiotherapy procedures are carried out).
An erroneous artery puncture was performed. (scheme to give) Stop manipulation, put a pressure bandage.
Possible damage to the needle of the median nerve in the ulnar fossa. (scheme to give)
Professional responsibility
All nurses who perform venipuncture undergo special training and practice under the guidance of an experienced supervisor, which should be properly documented. Their duty is to constantly raise the level of not only their theoretical knowledge and practical skills. The medical staff must act in accordance with the protocol / recommendations adopted in this medical institution.
The algorithm is the implementation of intravenous injection.
purpose
Indications
Prescribing doctor.
Contraindications
Defined by a doctor.
Injection site
Equipment
Possible patient problems that you may encounter during the procedure
The refusal of manipulation is usually due to previous negative personal experience or information about the presence of the development of various complications received from other people or patients.
Psychological discomfort associated with a feeling of fear, due to the soreness of the injection
Fear of possible infection
Fear of an allergic reaction
Fear of hematoma
Fear of mistaken drug administration
Fear of deterioration of the patient during the injection.
Performing a manipulation
Specify whether the patient had previously met with this procedure:
if so, for what reason and how did he transfer it?
if not, it is necessary to explain to the patient the essence of the procedure.
Get the patient's consent to the procedure.
Wash your hands.
Give the patient a comfortable position (supine or sitting) at which the intended injection site is well accessible. Ask the patient to free her from clothing.
Prepare the necessary equipment. Pay special attention to the absence of air in the syringe and needle penetration. To do this, place the syringe strictly vertically, at eye level. Pressing with the left hand on the piston, it is necessary to force the air out until the first drop of the medicinal solution appears.
By inspection and palpation, determine the immediate location of the upcoming injection.
Place an oil bag under the patient’s elbow.
Put on a mask
Wear gloves (if they are already worn - treat them with a cotton ball moistened with alcohol).
Put the tourniquet in the middle third of the shoulder (on the shirt or napkin), so that its free ends are directed upwards and the loop down (the pulse on the radial artery should not change!)
when using a special venous cuff, you must snap the valve on it and pull the free end until the venous blood flow stops.
Have the patient squeeze and unclench his fist several times, and then clamp it. Palpate the vein, determining its width, depth, direction, mobility, presence of wall seals.
Treat the area of the elbow with cotton balls moistened with alcohol. Move the ball in one direction - from the periphery to the center. The first ball needs to handle the area of the elbow bend, the second ball needs to handle the injection site directly.
Take the syringe in your right hand: the index finger fixes the needle cannula, the others cover the cylinder of the syringe. photo to do
In the course of the selected vein with the thumb of your left hand, pull the skin to the periphery and press it. Without changing the position of the syringe in the hand and keeping the needle cut up at an angle of 30 °, puncture the skin and insert the needle 1/3 the length parallel to the vein.
Continuing to fix the vein with the left hand, slightly change the direction of the needle and gently puncture the vein until the feeling of "falling into the void" appears. Secure your right hand with a syringe in this position.
You need to make sure the needle is in vein. To do this, move the left hand to the plunger and pull it towards you if blood appears in the syringe, therefore the needle is in vein and you have achieved the result you need.
Dissolve the harness with your left hand, pulling at one of the loose ends. Ask the patient to unclench
when using the venous cuff, press the lock valve with your left hand.
Without changing the position of the syringe, move your left hand to the piston. Clicking on it, slowly enter the medicinal solution. During pressure with the left hand on the piston, the position of the right hand must be firmly fixed.
During the procedure, you must constantly monitor general condition the patient and the state of the injection site during the administration of the solution.
At the end of the drug administration, it is necessary to press the ball moistened with alcohol to the injection site, remove the needle and bend the patient's arm at the elbow joint. Ask the patient to keep his arm bent for at least 5 minutes, then store the cotton ball in a container with a disinfectant or in a bag from under a disposable syringe.
Put the syringe in the tray, close the disposable needle cap, observing the universal rules of precaution.
Take an interest in the patient's well-being.
The end of the procedure. It is necessary to carry out decontamination of the used tools:
Rinse the syringe with the needle in
disinfectant solution;
Soak the syringe, needle, cotton balls in separate containers;
Take off the gloves and soak in a disinfectant solution.
Dispose of appropriate tools.
Make the necessary entry in the medical record.
Intravenous drip medication
purpose
Introduction of medicinal substances in the provision of emergency care
The introduction of drugs whose action is more effective when administered intravenously.
Indications
Prescribing doctor.
Contraindications
Defined by a doctor.
Place the needle into the vein
Elbow veins insert photo elbow
Veins forearm
Veins of the back surface of the brush insert photo
Veins of the temporal region (in children and infants).
Necessary equipment
Sterile disposable system for dropping liquids;
medicinal substance
vials with infusion solutions;
sterile trays;
sterile cotton balls,
70% alcohol solution in a bottle,
venous harness;
oilcloth cushion;
sterile gloves;
adhesive plaster;
bix with sterile dressing;
stand for fixing disposable system
bottle with 0.5% solution of ammonia.
disinfectant solution containers.
container for recycling needles, disposable syringes, disposable systems
Algorithm of the manipulation
See the beginning of the algorithm for intravenous injection. Further:
Open the bag and place the system in a sterile tray.
Remove the cap from the needle of the air duct. Insert the needle all the way into the stopper of the vial and fasten the free end of the duct along the vial (this can be done with a rubber band). Remember that in some systems, the air inlet is directly in the drip. In this case, you need to open the cap that closes this hole.
Close the clamp, remove the cap from the needle at the short end of the system and insert it into the stopper of the vial.
Turn the bottle over and secure it to the tripod. Turn the dropper filter in a horizontal position, open the clamp, slowly fill the dropper to half the volume. You can fill the dropper without turning it through 90 °, but simply pushing on its body 2-3 times so that the filter is completely immersed in the fluid for infusion.
Close the clamp and return the dropper to its original position. The filter must be completely immersed in the infusion fluid.
Remove the cap from the injection needle. Open the clamp and slowly fill the tube until the air is completely displaced and droplets from the injection needle appear, close the clamp. Put the cap on the needle. If you are filling the system without putting on a needle for injection, then drops of liquid should appear from the connecting cannula of the system.
Check for air bubbles in the system tube.
Put cotton balls moistened with a 70% alcohol solution and a sterile napkin in a sterile tray. Prepare and place on the upper part of the rack two strips of narrow (1 cm) adhesive plaster with a length of 4-5 cm.
Help the patient to take a comfortable position, lying on his back. Place an oilcloth under the patient's elbow.
Wear a mask.
Wear gloves (if they are already worn, they must be treated with a cotton ball moistened with alcohol).
Apply the tourniquet in the middle third of the shoulder (on the shirt or napkin) so that its free ends are directed upwards and the loop down (the pulse on the radial artery does not change!).
Ask the patient to squeeze and unclench his fist several times, and then clamp it. To palpate a vein, determining its width, depth, direction, mobility, presence of wall seals.
Treat the area of the elbow with cotton balls moistened with alcohol. The movement of the balls to carry out in one direction - from the periphery to the center. The first ball to handle the area of the elbow bend, the second - directly to the puncture site.
Take the needle with the right hand for the cannula, the left to remove the cap. Needle cutting should “look” at the nurse.
In the course of the selected vein with the thumb of the left hand, tighten the skin to the periphery and press it. Holding the needle upwards at an angle of 30 °, puncture the skin and insert the needle 1/3 the length parallel to the vein.
Continuing to fix the vein with the left hand, slightly change the direction of the needle and gently puncture the vein until a feeling of "falling into the void" appears. Note: you can use the single-step method, simultaneously puncturing the skin and underlying vein.
When blood appears in the system with his left hand, untie the tourniquet by pulling on one of the loose ends. Ask the patient to unclench his fist. Note: when using the venous cuff, press the lock valve with your left hand.
Open the clamp. Adjust the rate of dripping with a screw clamp according to the doctor's prescription.
Secure the needle with a plaster and cover it with a sterile cloth.
Take off the gloves. Wash your hands.
Observe the patient throughout the entire drip.
Wear gloves. Close the screw clamp when a small amount of solution remains. Note: when administering medicinal solutions from several bottles, it is necessary to do the following: when a small amount of solution remains in the first bottle, close the screw clamp, remove the air duct from the bottle and insert the second bottle in the stopper, which was previously mounted on a tripod. Also quickly move the needle to attach to the bottle on the short part of the system and open the screw clamp. Adjust the rate of flow of drops.
Press the ball moistened with alcohol to the injection site, remove the needle and bend the patient's arm at the elbow joint. Ask the patient to keep the arm bent at the joint for at least 5 minutes.
Close the needle system cap, observing the universal rules of precaution.
Make sure that the bleeding has stopped and put the cotton ball in a container with disinfectant or in a tray for used instruments.
Ask the patient how to feel. Make sure that he feels satisfactory.
End of procedure:
Disconnect the needle from the system. Place the system for intravenous drip infusion into the disinfectant solution. Cut the system into several parts and disinfect and dispose of them. Disinfect and discard the needle and cotton balls in separate containers.
Take off the gloves and soak in a disinfectant solution. Wash the hands. Dispose of gloves.
Record the procedure and patient response.
Treatment of harmful alcohol addiction is a difficult task. Sometimes doctors offer psychological coding, or you can inject alcoholism into a vein or under the scapula. This is one of the most effective ways to get rid of craving for alcohol. Specialists inject drugs for coding for intravenous alcoholism, and this is an important component of drug therapy. The doctor must prescribe it. The patient is warned about the possible consequences of drinking, consent is required in writing.
What is a shot from alcoholism
Antialcoholic injections are necessary for administering a drug intramuscularly or intravenously in order to quickly treat alcoholism. Effective drug in the body for a long timetherefore, the relatives of the alcoholic may not worry about the patient’s state of health. This is an alternative to any kind of encoding. It provides several ways to administer the drug.
Injection principle
Medicinal substances in the composition of injections interact with any alcoholic beverage, causing acute symptoms of intoxication, pronounced signs of dyspepsia, and food poisoning. Therefore, the use of alcoholic beverages is strictly prohibited, only in this case, the drug will not give side effects.
This is partly a psychological effect on an alcoholic who is first explained the possible consequences of intravenous and intramuscular injections. If to refuse the use of alcoholic drinks, and then to break the promise, it is possible to risk strongly.
What effect do alcohol shots cause?
After the injection in a sober state, nothing happens, and the patient can live a full life. The basic rule is to forever refuse to drink alcohol.. Otherwise, you can feel the medical impact of the synthetic components of the injection. If an alcoholic violates the basic rule and drinks alcohol again, the following symptoms await him after a single dose:
- signs of food poisoning;
- nausea, vomiting;
- muscle cramps;
- bouts of tachycardia, arrhythmias;
- blood pressure surges;
- migraine attacks;
- lack of appetite.
How many times can be coded from alcohol addiction
For the treatment of alcohol dependence, this method can only be used for medical reasons. For example, in case of liver diseases, it is better to find another "file", otherwise, at the next breakdown, you can remain disabled or even completely die. With the help of injections intravenously or intramuscularly, it is possible to encode more than once, but each time after the injection is injected, the therapeutic effect weakens, the duration of the coding period is reduced.

Alcohol Coding Products
Procedures are carried out by specialists in the hospital after preliminary medical examination. The choice of medication does not depend on the dose of alcohol, but on the characteristics of the organism, the presence of chronic diseases. Therefore, when coding it is important not to start from the positive reviews of friends, but from the instructions for use, the recommendations of the attending physician. Below is a table explaining what an injection is done when coding for alcoholism in the hospital.
| drug name
| mechanism of action
| complications
| price, rubles
|
| Disulfiram
| Disulfiram is injected into a vein, the drug acts from 1 to 3 years. Disulfiram injections are not performed for serious illnesses.
| Severe migraine attacks, memory disorders, angina, brain swelling.
|
|
| Algominal
| The active ingredient disulfiram produces enzymes in the liver that prevent the breakdown of ethanol. It increases its concentration in the blood.
| Pressure drops, angina, tachycardia, pressure drops, fainting.
| 3,000 (for 3 months)
|
| Vivitrol
| Intramuscularly, help to cause acute attacks of intoxication, impaired stool. Able to block opioid receptors.
| Nausea, vomiting, anorexia, abdominal pain, signs of dyspepsia.
|
|
| Delphison
| The injection is performed intramuscularly, causes side effects after drinking a dose of alcohol.
| Extensive pathology of the cardiovascular system, blood-forming organs.
|
|
|
| After the injection, you can not drink alcohol, otherwise the dose of ethanol in the blood is pathologically increased.
| Symptoms of intoxication, tachycardia and heart rhythm disturbances.
|
|
| Esperal gel
| Intramuscular injection, prevents drunkenness due to the activity of active substances. When interacting with ethanol, the drug blocks the nerve endings and causes signs of food poisoning.
| Lack of appetite, signs of dyspepsia, internal weakness, instability of the stool.
|
|
|
| The active ingredients increase the toxicity of alcoholic beverages, deliberately poison the body.
| Complete intoxication of the body, dehydration.
|
|
Types of injections
For alcoholism, medications are administered in three ways: in the liver, intravenously and intramuscularly. In the latter case, the therapeutic effect is weaker, it is considered one of the not the most reliable methods of getting rid of alcohol dependence. To code an alcoholic, you need to contact a specialist clinic, where the doctor injects the medicine through a syringe into a vein or liver.

Intravenous coding
Intravenous injection used in complicated clinical situations where the chronic alcoholic needs immediate results. It is considered the injection enters directly into the blood in a high concentration, which does not decrease for a long period of time. When reactions with ethanol provokes extensive symptoms of intoxication. Injections into the vein are held in a specialized clinic, the usual means are valid for a year. Disulfiram is often administered, which provides coding from alcoholism for injection into a vein from 1 to 3 years.
Intramuscular injections
This is the safest technique that has mild side effects. It is possible to make an injection from alcoholism at home, and among the most popular are the drugs Vivitrol and Esperal at a price of up to 8,000 rubles. Such medications are used when the health problem is not yet global, and verbal conviction affects the patient.
Subcutaneous injection
The most popular method is the Torpedo, when the ampoule with the drug is injected subcutaneously (stitched). The price of the drug is affordable, but the therapeutic effect is weak, and many alcoholics, without fear for their health, return to drinking alcohol. So that a dependent person at home doesn’t seize Torpedo on his own (not decoded), the ampoule is sewn under the paddle, from where it is harder to remove.
Spade Coding
With this pharmacological appointment we are talking about a special gel of homogeneous consistency, which is encapsulated after several days, general hyperthermia is manifested. The procedure is called behind the scenes "tamping", accompanied by pain and internal discomfort. Injecting the drug is indicated only in the hospital, its cost is available, but the effect in the body is short. More often used stronger and faster injections from alcoholism.
Hot injection to the liver
To ensure a quick effect, you can directly act on liver enzymes.. A hot injection from alcoholism works according to this principle: after the injection, the active components block the process of ethanol disintegration, which increases its concentration in the blood. In the body, poisoning occurs so that the alcoholic will experience strong side effects and later he feared to drink again. The procedure is carried out by a specialist, the therapeutic effect for several months.
How much does the alcohol coding hold
The effectiveness of the injection of alcoholism is determined individually. If this drug Aquilong, the therapeutic effect weakens after six months, requires the introduction of another dose. But the anti-alcohol efficacy of Dsulfiram varies from 1 to 3 years. It is advisable to choose a medicine so that its therapeutic action lasts for a year, and then, if necessary, repeat the procedure.
Side effects and contraindications
Like any treatment, this method has a number of contraindications. The use of alcoholism injections is prohibited when:
- nervous disorders;
- pregnancy;
- abstinence;
- extensive liver damage;
- cardiovascular pathologies;
- infectious diseases compensation stage;
- organic brain lesions.
Side effects during therapy may be as follows:
- severe signs of dyspepsia;
- disorders of the cardiovascular system;
- confusion;
- drops in blood pressure;
- fainting, migraine attacks.
Injection Coding - Efficacy and Effects
If, after coding, to take a dose of alcohol, the patient begins to feel sick and vomiting. These are obvious symptoms of intoxication of the body, which have different intensity depending on the drug used and the drunk dose of alcohol. To enhance the effectiveness of treatment, a double encoding from alcoholism is necessary - the injection of the injection in combination with psychological training.
Video
The Princess line of intradermal fillers, which include non-animal stabilized hyaluronic acid, is a new generation of products aimed at correcting the signs of age-related skin changes. They are designed for contouring and biorevitalization procedures, they are distinguished by a high degree of safety, the lowest possible development of side effects and excellent results in the fight against skin aging.
The line of homogeneous, highly elastic dermal fillers of the new generation Plüreal (Pluryal), prepared on the basis of hyaluronic acid, allows you to quickly and painlessly smooth wrinkles and stop the aging process of the skin.
Every day new products appear on the market of cosmetic products that help stop the aging process of the skin and preserve its youth and beauty, and this includes innovative medicine for mesotherapy - Konzhaktil, produced by the French company Sedifa Laboratoire. Indications for use, efficacy and benefits of the drug.
The first successful attempts to rejuvenate the skin by intradermal injection of drugs prepared on the basis of embryonic cells of animal origin - organ tissue therapy, were carried out at the end of the XIX century. Since then, this area of aesthetic medicine has been actively developing and today the procedure of injecting skin rejuvenation by the French drug, Embryoblast from the Filorg Laboratory (FILORGA), is popular among cosmetic clinics clients.
The line of dermal fillers and biorevitalizants Apriline, which include hyaluronic acid, obtained using the unique stitching technology - A.P.R.I, is a new generation of anti-aging products. What are the benefits of gels in this series?
One of the main tools that modern, dynamically developing anti-aging medicine uses is hyaluronic acid-based preparations - fillers. Procedures such as removing bags under the eyes, removing wrinkles, correcting the shape of the nose, increasing the volume of the lips, non-surgical facelift and even skin rejuvenation are not without them.
How can an ordinary consumer understand this diversity and make right choice? Which dermal filler is the best? Which filler will give the best result? Which one is the most gentle and safe, and which one has the most resistant action?
Stylage (Stylage®) - filler, which due to its characteristics is rapidly gaining popularity not only in the French market. Since it contains mannitol, the risk of redness and swelling after injection is lower than with other drugs. Mannitol neutralizes hydroxyl radicals that are released during intradermal injections.
Revofil is a line of effective drugs for biorevitalization and contour plastics that can slow down skin aging processes. The unique composition of intradermal gels allows for a short time to moisturize the skin, smooth mimic wrinkles and provide a lifting of soft tissues, and innovative production technology makes the procedure with their use absolutely safe for the patient.
With intramuscular injection, medicinal substances are injected into the muscle layer, located below the subcutaneous fatty tissue. Muscles are less sensitive than skin and subcutaneous fat. Medicines injected into them are absorbed faster due to the greater number of vessels and muscle contraction. Intramuscularly injected many drugs that are available in solutions and do not cause irritation of soft tissues. If you need to enter 2 drugs, they should be checked for compatibility. With their incompatibility, different syringes are used and drugs are injected in different places. If it is necessary to carry out a series of injections, the injection sites must be changed and recorded. This reduces the likelihood of local tissue reaction and improves the absorption of the drug. For some patients, intramuscular injections are contraindicated (for example, for persons with poor blood clotting).
Intramuscular injection can be executed in the shoulder area (deltoid muscle), in the middle third of the anterior anterior surface of the thigh (broad lateral muscle of the thigh) and in the buttocks (upper outer quadrant of the buttock). The area of the upper outer quadrant includes large, medium and small gluteal muscles. Intramuscular injections are most often performed in the gluteal muscles. The zone suitable for injections can be set along bone landmarks, mentally drawing a vertical line through the ischial tubercle, and a horizontal line through a large twist of the femur. Thus, the gluteal region is conventionally divided into 4 parts. Intramuscular injection can only be done in the upper outer quadrant. It is impossible to inject into the upper inner quadrant, since the sacrum occupies most of the quadrant, and the muscle layer is very small here. In the inferior quadrant, there is a large artery, vein and sciatic nerve, in the inferior quadrant most of it is occupied by the femoral head.
When determining the injection site, the patient may lie:
a) on the stomach, with the toes of his legs turned inward;
b) on the side with the leg, which will be on top, bent at the thigh and knee to relax the gluteus maximus.
Intramuscular injection can also be carried out in the lateral broad muscle of the thigh, which is well developed and is the preferred injection site not only in adults, but also in children.
To determine the injection site on the thigh, the nurse places her right hand 1-2 cm below the spit of the femur, the left one 1-2 cm above the patella, the thumbs of both hands should be on the same line. The injection site is located in the center of the area formed by the index and thumbs of both hands.
When performing injections in young children and infirm adults, skin and muscle should be taken into a fold to be sure that the drug has hit the muscle.
The position of the patient with this injection is supine with a leg slightly bent at the knee, into which the injection will be made, or sitting.
Intramuscular injection can also be performed in the deltoid muscle. Sisters rarely use this area for injections — only when other places are unavailable or when several intramuscular injections are performed daily. It should be remembered that in children this muscle is poorly developed.
To determine the injection site in the deltoid muscle, you can ask the patient to release the shoulder and shoulder blade from the clothes. The patient's arm is relaxed and bent at the elbow. During the injection, the patient may lie down or sit. The injection site is determined by attaching four fingers across the deltoid muscle, starting from the acromion process.
Intramuscular Injection Technique
Prepare: a syringe with a solution of the drug substance and a needle for intramuscular injection, sterile cotton balls, alcohol 70 °, rubber gloves.
1. Take the syringe in your right hand, “like a pen,” the second finger on the needle cannula, the first and third fingers on the cannula rim of the cylinder.
2. With your left hand, palpate the injection site so that there is no infiltration.
1. In the left hand, take the alcohol ball and process the skin from the top down twice, first 10x10 cm, and then 5x5 cm.
2. Hold the ball under the fifth finger of your left hand.
3. The first and second fingers of the left hand stretch the skin in the injection area, without touching the area of not mediocre drug administration.
4. Holding the syringe perpendicular, at a 90 ° angle, insert the needle into the muscle to a depth of 2/3 of the needle.
7. Transfer the left hand to the plunger of the syringe and slowly slowly insert the drug.
8. Apply a cotton ball to the puncture site with the second finger of your left hand. Remove the needle with a quick movement.
9. Ask the patient to hold the cotton ball for 5 minutes without rubbing.
10. Place a cotton ball and a needle in separate containers with a disinfectant solution. Place a cotton ball in a 3% solution of chloramine for 1 hour. Free the syringe from the residual blood in tank No. 1 and disassemble it in disassembled container No. 2.
Note.Subcutaneous and intramuscular injections can be done without intercepting the syringe in your left hand, and you can inject the medicine with your left hand.
Some doctors believe that in the treatment of acute anaphylaxis, intramuscular administration of corticosteroids is more effective than oral administration. This assumption seems to be based on an analogy with intramuscular injection adrenaline with anaphylaxis. However, to date there are no convincing scientific data proving the advantages of such tactics over oral administration of corticosteroids.
Vitamin B 12
Until recently, the standard therapy for vitamin B12 deficiency was its exceptional intramuscular administration. (31 - 35) This practice was based on scientific evidence indicating that when malabsorption of vitamin B12 (internal factor Casla deficiency), the intestine is able to absorb only 1-2% of vitamin B12 ingested. (32 - 35). However, in recent years, several studies have been conducted that have suggested treating such patients with high doses of oral vitamin B12. (31 - 35)
These studies have shown that the effectiveness of oral high-dose therapy with vitamin B12 is not inferior to its intramuscular administration in the short term. (31–35) In one study, vitamin B 12 was orally administered at a dose of 2,000 mg per day for four months. (36) This led to a threefold increase in the level of serum vitamin B12, compared with the monthly rate of injections of vitamin B12. However, other studies in which vitamin B12 was administered orally at doses of less than 500 micrograms per day did not achieve the desired result, which confirms the need for daily administration of precisely high doses of the drug. (37, 38) It should be noted that there are no studies to compare the long-term results of the effectiveness of the intramuscular and oral routes of administration of vitamin B12 in the treatment or prevention of anemia.
There are several reasons why oral administration of vitamin B12 should be preferred to intramuscular administration. First, injections require hospital visits, which can be difficult for patients with reduced mobility and elderly patients. Secondly, injections are accompanied by a higher incidence of complications and injuries. (31 - 35) Thirdly, the injections of this drug are very painful. Ingestion of vitamin B12 is a painless, effective, safe, cost-effective and technically convenient form of administration of the drug, suitable for most patients. (31–33)
Ketorolac
All NSAIDs (NSAIDs, nonsteroidal anti-inflammatory drugs) have the same mechanism of action, regardless of the route of administration. (39 - 41) Modern scientific studies do not find the advantages of intramuscular administration of Ketorolac over its oral intake, for such diseases as migraine, gout, musculoskeletal pain, etc. (40 - 43) Several studies that compared oral ibuprofen with intramuscular ketorolac did not find significant differences in efficacy. (40 - 43)
In addition, studies failed to prove the hypothesis that intramuscular ketorolac is a more effective treatment for renal colic than oral NSAIDs. (44, 45) Limited studies have even shown that intramuscular ketorolac has the same effect as some opioids in treating renal colic. (40, 41, 44, 45). It should be said that so far there are no randomized, double-blind studies that would directly compare oral NSAIDs with intramuscular ketorolac.
The negative aspects associated with the intramuscular administration of Ketorolac include: bruising, local infections, hematomas, patient discomfort, and injuries from a needle. (38, 39) In addition, intramuscular NSAIDs are much more expensive than oral. (39, 42) Given the lack of evidence of the benefits of intramuscular NSAIDs over oral NSAIDs, intramuscular preparations should be used only for patients with acute pain, as well as those who are not able to take the drugs by mouth. (39 - 42)
Conclusion
Due to the wide nature of this topic, we have limited ourselves to comparing the intramuscular and oral routes of administration. In addition, drugs such as antihistamines, opioid analgesics, ondansetron, triptans, and many others were not included in the review. It is hardly possible to develop strict criteria for choosing the route of administration of these drugs. The process of making choices should be individualized, include an assessment of the clinical picture, knowledge of the properties of drugs and consideration of patient preferences. With rare exceptions, there is no evidence that intramuscular drugs act more quickly or more efficiently than oral ones. Therefore, practitioners should in most cases give preference to the oral route of administration of drugs.
Bibliography - Reeler AV. Anthropological perspectives on injections: a review. Bull World Health Organ. 2000; 78 (1): 135-143.
- Kienle GS, Kiene H. The powerful placebo effect: fact or fiction? J Clin Epidemiol. 1997; 50 (12): 1311–1318.
- Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases of the Commonwealth of America / American Thoracic Society, acquired pneumonia in adults. Clin Infect Dis. 2007; 44 (suppl 2): S27 – S72.
- Chang EJ, Marcy SM. Intramuscular antibiotics in the treatment of pediatric upper respiratory tract infections. Am J Manag Care. 1999; 5 (15 suppl): S915 – S922.
- Wong DM, Blumberg DA, Lowe LG. Guidelines for acute respiratory infections. Am Fam Physician. 2006; 74 (6): 956–966.
- Stevens DL, Bisno AL, Chambers HF, et al., For the Infectious Diseases Society of America. Practice Guidelines for Skin Care and Soft-tissue Infections. Clin Infect Dis. 2005; 41 (10): 1373–1406.
- Pohl A. Modes of antibiotics administration for symptomatic severe urinary tract infections.Cochrane Database Syst Rev. 2007; (4): CD003237.
- Baker PC, Nelson DS, Schunk JE. In addition, patients with urinary tract infections do not improve outcome. Arch Pediatr Adolesc Med. 2001; 155 (2): 135–139.
- Hoberman A, Wald ER, Hickey RW, et al. Oral versus initial intravenous therapy for children. Pediatrics. 1999; 104 (1 pt 1): 79–86.
- Roberts KB. AAP practice parameter for infants and young children. American Academy of Pediatrics. Am Fam Physician. 2000; 62 (8): 1815–1822.
- Green SM, Rothrock SG. Single-dose intramuscular ceftriaxone acute otitis media in children. Pediatrics. 1993; 91 (1): 23–30.
- Barnett ED, Teele DW, Klein JO, Cabral HJ, Kharasch SJ. Comparison of ceftriaxone and trimethoprim-sulfamethoxazole for otitis media. Greater Boston Otitis Media Study Group. Pediatrics. 1997; 99 (1): 23–28.
- Varsano I, Volovitz B, Horev Z, et al. Intramuscular ceftriaxone compared with oral amoxicillinclavulanate for treatment of otitis media in children. Eur J Pediatr. 1997; 156 (11): 858–863.
- Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. http://www.cdc.gov/std/treatment/2-2002TG.htm. Accessed August 22, 2008.
- Bisno AL, Gerber MA, Gwaltney JM Jr, Kaplan EL, Schwartz RH. Streptococcal pharyngitis. Infectious Diseases Society of America. Clin Infect Dis. 2002; 35 (2): 113-125.
- Centers for Disease Control and Prevention. CDC changes recommendations for treatment resistance. Accessed August 22, 2008.
- Ross J. Pelvic inflammatory disease. Clin Evid. 2006; (15): 2176–2182.
- Institute for Clinical Systems Improvement. Health care guideline: diagnosis and management of asthma. Accessed September 2, 2008.
- U.S. Department of Health and Human Services. ASTRAHMA EDUCATION PROGRAM Accessed August 22, 2008.
- Dennis R, Solarte I, Fitzgerald JM. Asthma Clin Evid. 2005; (14): 1847-1877.
- Rowe BH, Spooner C, Ducharme FM, Bretzlaff JA, Bota GW. Early emergency department treatment with asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001; (1): CD002178.
- Rowe BH, Spooner CH, Ducharme FM, Bretzlaff JA, Bota GW. Corticosteroids for preventing relapse of the following acute exacerbations of asthma. Cochrane Database Syst Rev. 2000; (2): CD000195.
- Lahn M, Bijur P, Gallagher EJ. Randomized clinical trial of oral methylyprednisolone in the treatment of asthma exacerbations following discharge from an emergency department. Chest. 2004; 126 (2): 362–368.
- Gries DM, Moffitt DR, Pulos E, Carter ER. A single dose of intramuscularly administered is to be taken in order to prevent asthma exacerbations in young children. J Pediatr. 2000; 136 (3): 298–303.
- Amir L, Hubermann H, Halevi A, Mor M, Mimouni M, Waisman Y. Oral betamethasone versus intramuscular viral croup: a prospective, randomized trial. Pediatr Emerg Care. 2006; 22 (8): 541–544.
- Rittichier KK, Ledwith CA. Outpatient treatment of moderate group with dexamethasone: intramuscular versus oral dosing. Pediatrics. 2000; 106 (6): 1344-1348.
- Bjornson CL, Klassen TP, Williamson J, et al., For the Pediatric Emergency Research Canada Network. A randomized trial of a mild croup. N Engl J Med. 2004; 351 (13): 1306-1313.
- de Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in a treatment of COPD exacerbations: a randomized, conrolled, double-blind study.Chest. 2007; 132 (6): 1741–1747.
- Razi E, Moosavi GA. A comparative efficacy of oral prednisone with intramuscular triamcinolone exacerbation of asthma. Iran J Allergy Asthma Immunol. 2006; 5 (1): 17–22.
- Drugs for allergic disorders. Treat Guidel Med Lett. 2007; 5 (60): 71–80.
- Andrès E, Federici L, Affenberger S, et al. B12 deficiency: a look beyond pernicious anemia. J Fam Pract. 2007; 56 (7): 537-542.
- Oh R, Brown DL. Vitamin B12 deficiency. Am Fam Physician. 2003; 67 (5): 979–986.
- Butler CC, Vidal-Alaball J, Cannings-John R, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: a systematic review of randomized controlled trials. Fam Pract. 2006; 23 (3): 279–285.
- Nyholm E, Turpin P, Swain D, et al. Oral vitamin B12 can change our practice. Postgrad Med J. 2003; 79 (930): 218–220.
- Eussen SJ, de Groot LC, Clarke R, et al. Oral cyanocobalamin supplementation in older people with vitamin B12 deficiency: a dose-finding trial. Arch Intern Med. 2005; 165 (10): 1167–1172.
- Kuzminski AM, Del Giacco EJ, Allen RH, Stabler SP, Lindenbaum J. Effective treatment of cobalamin deficiency with oral cobalamin. Blood. 1998; 92 (4): 1191-1198.
- Lederle FA. Oral cobalamin for pernicious anemia. What’s best kept secret? Jama. 1991; 265 (1): 94–95.
- Rajan S, Wallace JI, Brodkin KI, Beresford SA, Allen RH, Stabler SP. Response of elevated methylmalonic acid to older levels of oral cobalamin in older adults. J Am Geriatr Soc. 2002; 50 (11): 1789-1795.
- Drugs for pain. Treat Guidel Med Lett. 2007; 5 (56): 23–32.
- Arora S, Wagner JG, Herbert M. Myth: parenteral ketorolac provides more effective analgesia than oral ibuprofen. CJEM. 2007; 9 (1): 30–32.
- Turturro MA, Paris PM, Seaberg DC. Intramuscular ketorolac versus oral ibuprofen acute musculoskeletal pain. Ann Emerg Med. 1995; 26 (2): 117–120.
- Schwartz NA, Turturro MA, Istvan DJ, Larkin GL. Patients ’selection of a route of nonsteroidal anti-inflammatory therapy. Acad Emerg Med. 2000; 7 (8): 857–861.
- Shrestha M, Morgan DL, Moreden JM, Singh R, Nelson M, Hayes JE. Randomized double-blind comparison of intramuscular ketorolac and oral indomethacin in the treatment of acute gouty arthritis. Ann Emerg Med. 1995; 26 (6): 682–686.
- Teichman JM. Clinial practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004; 350 (7): 684–693.
- Holdgate A, Pollock T. Systematic review of the relative efficacy of non-steroidal anti-inflammatory drugs and opioids in the treatment acute renal colic. BMJ. 2004; 328 (7453): 1401.